FORT WORTH, Texas, May 20, 2020 — CERIS, a division of CorVel Healthcare, and a leading national provider of payment integrity and prospective claims review for health care payers, now offers a dashboard for its insurance clients to provide up-to-date information regarding the number of COVID-19 cases, the location and the type of claim, allowing payers to make informed decisions regarding payment integrity processing.
As COVID-19 continues to evolve at a rapid pace, CERIS found that clients were unsure of how to move forward with payment integrity processing during the pandemic, especially in states with hotspots. Bill review was being put on hold across entire states, despite the fact that COVID-19 outbreaks are often localized and may not impact an entire state or county.
“It is important that we provide relief to hospitals that are overwhelmed due to the pandemic by reducing any extra work. However, we also understand that some hospitals haven’t been impacted as severely by the virus and accurate payment review could and should continue,” stated Corey Albrecht, President of CERIS. “The new dashboard provides accurate information to help our customers make informed decisions on a case-by-case basis, rather than make broad decisions based on assumptions.”
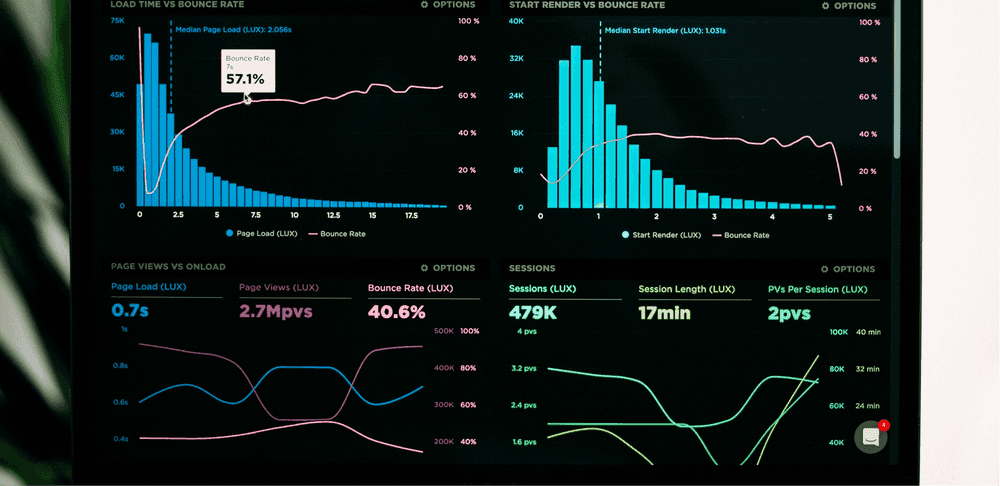
The COVID-19 dashboard provides clients with the ability to understand the status of cases on a daily basis, including the number of cases, where they are coming from, and how many claims have been reviewed through the payment integrity process. Payers can review detailed claim information across the country, at the state, county, or city level, or all the way down to an individual hospital. Detailed claim information provides clients with the data they need to make decisions regarding when to put bill review on hold for a particular hospital or region, versus shutting down the process across an entire state.
“We developed this solution because we view our responsibility to clients as being more than accurate and timely bill review—we have a responsibility to step up and guide our clients through challenging situations, like COVID-19, by providing detailed information to improve the decision-making process,” said Albrecht.
About CERIS
CERIS, a leader in both prospective and retrospective claims review and re-pricing, combines clinical expertise and cost containment solutions to ensure the accuracy and transparency in healthcare payments. Accuracy and validation services include itemization review, facility repricing, contract and policy applications, review of implants and devices, and primary payor cost avoidance. Its universal chargemaster contains billions of charge items from more than 97% of the nation’s hospitals, helping to ensure accuracy and objectivity of each claim review. On average, CERIS’ services achieve 62% savings on implant claims, 6% savings in network claims adjustments, and 35% savings on out of network claims adjustments.